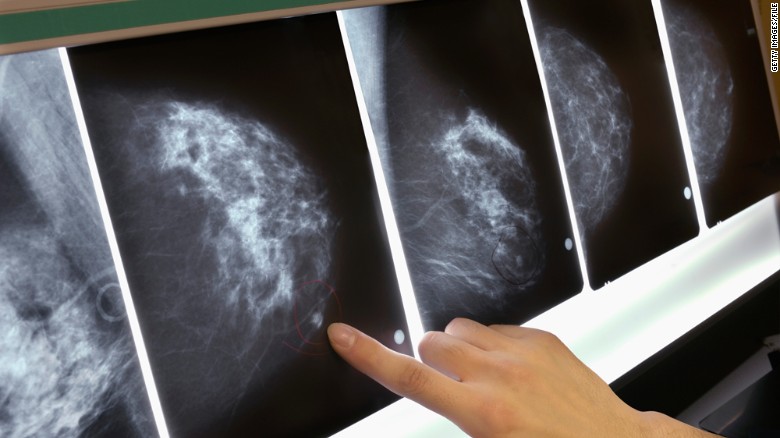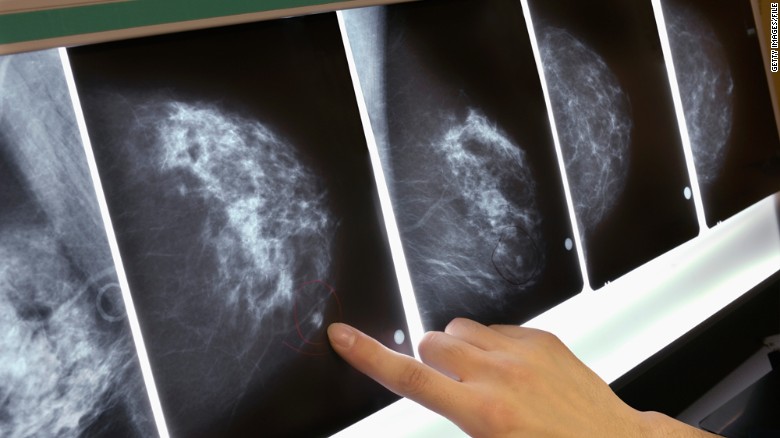
Canadian women should be outraged. The Canadian Task Force on Preventive Health (CTF) released its latest guidelines for screening for breast cancer for women at average risk. They advise against mammography for women aged 40 to 49, against women doing breast self-examination (BSE) and against doctors doing breast exams. They recommend women age 50 to 74 have mammograms every two to three years.
A 2014 study of screening in Canada showed 40 per cent fewer deaths among women who had screening mammograms than women who didn’t, but the CTF deliberately chose to ignore observational studies done with modern mammography equipment in favour of Randomized Control Trials (RCTs) from the 1960s to 1990s, which show only a 15 to 20 per cent mortality reduction.
The only measurable outcome of a RCT is how many women die of breast cancer, so the CTF ignores three other significant benefits of early detection of cancer: the ability to avoid mastectomy, lymphedema and chemotherapy.
How can the CTF not recommend annual mammography starting at age 40, if it saves the most lives and allows more women to have less aggressive treatment? The answer is they focus on “harms”: the number of women who are recalled for additional tests after screening and “overdiagnosis.”
About 10 per cent of women need additional tests after screening. The CTF uses the pejorative term, “false positive.” That term implies that a cancer was diagnosed when none was present. This is not the case: women are recalled when there is a potential cancer. This causes anxiety for many women, but it’s transient and studies show that it doesn’t harm women long-term.
The CTF gives undue weight to overdiagnosis in the harms-to-benefit discussion. Overdiagnosis is the theoretical possibility that a woman will be diagnosed with breast cancer and treated for it, but die of something else (like a heart attack) before she would have died of cancer. The rate of overdiagnosis can only be estimated. Experts estimate it at 10 per cent or less.
The CTF says that most women age 40 to 49 would choose not to be screened. From my thousands of conversations with women during my career and in published research, when told that mammograms can prevent breast cancer death, and allow them to have a lumpectomy and avoid chemotherapy if cancer is detected early, most women choose to be screened.
The CTF calls breast density an “emerging issue.” We’ve known about it for 40 years! Having dense breasts is a higher risk than having a mother or sister with breast cancer. Mammography is 96 per cent sensitive in fatty breasts, but only about 50 per cent sensitive in the densest breasts. And when cancers go undetected by mammography, they grow larger and can spread by the time they are found. The CTF has not acknowledged the harm of not offering supplementary screening for women with dense breasts.
The CTF says there’s insufficient evidence to recommend supplementary screening for women with dense breasts because of their insistence on RCTs. An RCT of screening ultrasound is underway in Japan but it will take at least seven to 10 years before it can prove mortality reduction. We have observational data from multiple studies showing that ultrasound finds an additional three to four cancers per thousand women.